Nurse-Led Innovation in Home Care - The H.O.P.E. Model™ of Care
Nurses make up nearly half of the regulated workforce in Canada’s healthcare system,(1) and recommendations from recent studies suggest that optimizing this group will be key for strengthening the healthcare system and providing better patient outcomes, particularly in the Home and Community Care sector.(2)
To innovate a model of care focused on empowerment and a healthy work environment for both nurses and patients, while addressing the growing number of aging Canadians who will require Home and Community Care in the coming years, one organization looked to their origins in primary nursing.

Drawing Inspiration From Primary Nursing:
SE Health is a national social enterprise and home health organization, with locations in most provinces across Canada. They got their start as a visiting nursing organization in the early-1900’s, with four core nurses providing around-the-clock care for nearly 1000 patients.
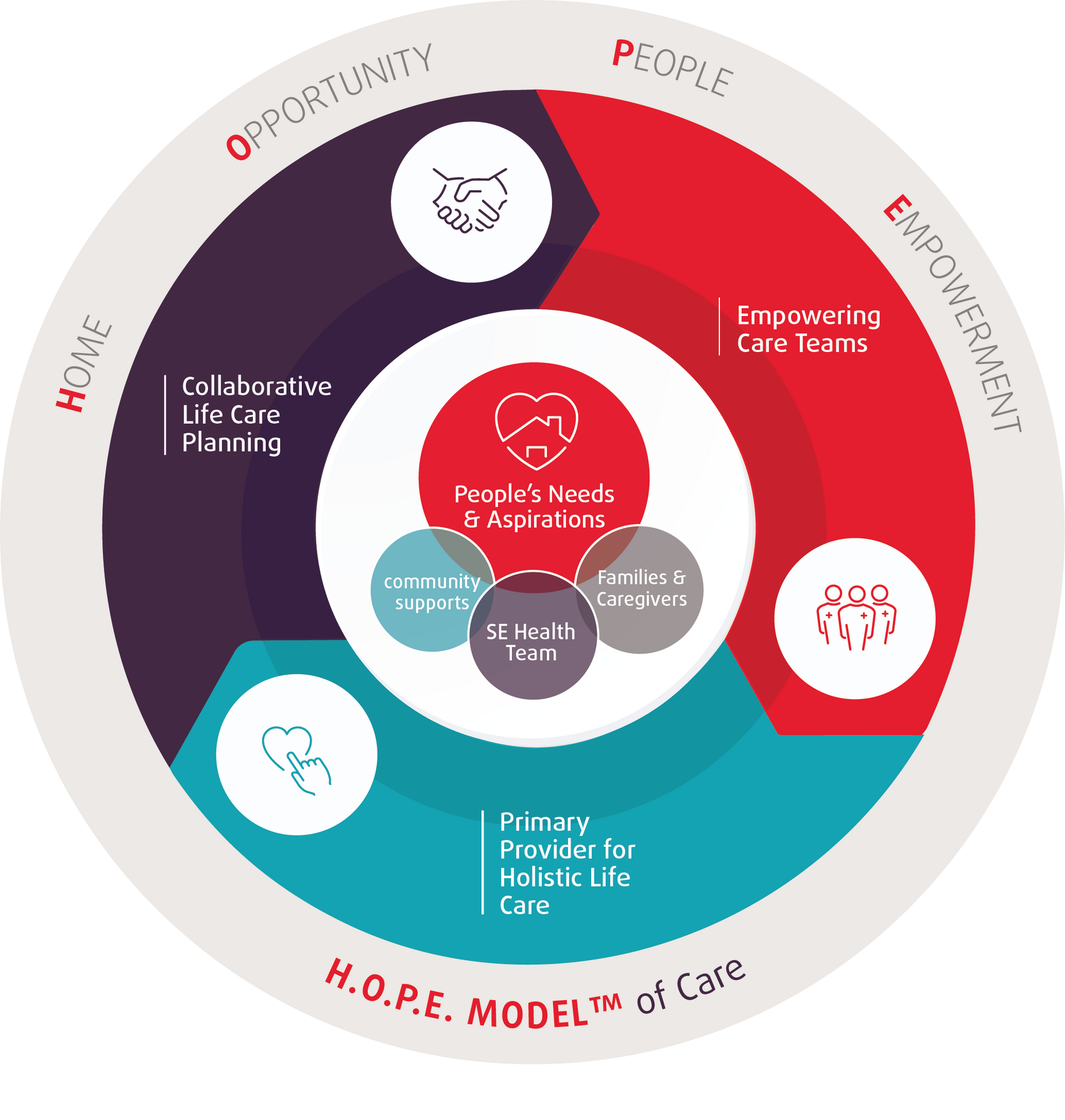
Taking inspiration from their history, as well as the Dutch Buurtzorg model, in which self-governing nursing teams provide a range of medical and home care services to a small roster of patients within their designated neighbourhoods,(3) SE Health developed the H.O.P.E. (Home, Opportunity, People and Empowerment) Model™, as a way to modernize home care and to improve patient experience and outcome.
Although home care is publicly funded in Ontario, many patients end up using a mix of public services and additional private services paid out of pocket.(4) Additionally, home care providers say the referrals they receive can be task-specific, making for a patchwork of care from different providers.
An example, says Kaiyan Fu, Vice President, Senior’s Health & Chief Clinical Executive at SE Health, is a client SE Health previously had on their service to receive antibiotics for wound infections, who had more than ten different nurses in and out of her home for care provision. “So there would be a high chance of miscommunication between all of these different nurses going in and out, the continuity was not there, and it introduced the likelihood of risks for care delivery,” Fu says.
Conversely, under the H.O.P.E. Model™ with one primary nurse accountable for the client holistically from admission to discharge, there would be a comprehensive care plan and consistent care delivery for better patient outcomes. “More importantly, through technology, through regular team huddle or communication, the primary nurse and the partner nurses would be all on the same page to meet the client's care needs,” says Fu.
The H.O.P.E. Model™ in Practice:
SE Health started developing the H.O.P.E. Model™ proof of concept in 2016, with a team of four nurses and just a handful of clients. The concept is that clients are assigned to a primary nurse, who, through self-directed scheduling, oversees and provides the majority of their home care services, integrating community and social services as needed. Partner nurses make it possible to access services around the clock, while maintaining consistency of care. “It is truly a nurse-led model, from design to implementation,” says Fu.
Patients are involved in guiding their own care plans, which include non-medical influences on their overall health. “If we design the health system from the perspective of a patient lying in a hospital bed, with their current health issues and limitations, we end up with a very different system than if we were to design it from the starting point of where the person is in their home, with the support of their network and community resources,” Shirlee Sharkey, former CEO of SE Health, writes in the H.O.P.E. Model™ proof of concept, “Leadership Perspective: Bringing Nursing Back to the Future Through People-Powered Care,” co-written with Nancy Lefebre, Chief Operating Officer at SE Health.(5)

Using implementation science, specifically, the i-PARIHS framework, SE Health has started to adapt and localize the H.O.P.E. Model™ within their current system and needs, in addition to using it to inform how they approach care at an organizational level. This organizational transformation is referred to as H.O.P.E. Approach to Care.
Fu says the feedback from clients and nurses has been positive. “We have been hearing from our nurses that one of the several reasons that they're passionate about home care, is that therapeutic relationship,” something that is much harder to establish in acute care, which is more episodic, she says. “But in home care, that relationship can be much longer through a person-centred focus. So through this model, we are actually seeing over the last couple of years, starting to turn things around in terms of the retention of our nurses. So that is a significant cost savings at a system level.”
Nurse-Developed Technology:
Rethinking their approach to home care, also meant exploring how technology could facilitate a more holistic experience for nurses and patients.
“We did a discovery journey map of the nurses’ experience and we said, ‘Wow, they've been interacting with more than 25 different platforms,’” says Sarah Tam Lee, Clinical Director, Practice Transformation at SE Health, “And that could be through messaging, [Microsoft] Teams, emails, phones, different web applications, and they describe that it’s quite burdensome to be able to interface with so many applications.”
They tasked a group of nurses with designing a digital application, the MySE Life app, and managed to decrease the amount of interfaces down to less than 11. “And we're continuing to try to decrease that even further, to make that more streamlined,” says Tam Lee, “So that particular tool really helps empower [nurses] with informed decision making, giving them the information about a client to help with planning and coordination, and allowing them to deliver really great care.”
This entrepreneurial spirit of healthcare professionals has always existed, Fu says, “It’s the intentional emphasis in enabling and empowering nurses for care delivery, practice ownership and innovation.”
References
- Backgrounder: 70 years of RN effectiveness [Internet]. Toronto (CA) Registered Nurses’ Association of Ontario, 2018 [cited 2023 Jun 28]. [5 pages]. Available from: https://rnao.ca/sites/rnao-ca/files/Backgrounder-_RN_effectiveness.pdf
- Ganann R, Weeres A, Lam A, Chung H, Valaitis R. Optimization of home care nurses in Canada: A scoping review. Health Soc Care Community [Internet]. 2019 [cited 2023 Jun 27]. 27(5):e604– e621. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/hsc.12797 doi:10.1111/hsc.12797
- Gray B, Sarnak DO, Burgers J. Home Care by Self-Governing Nursing Teams: The Netherlands' Buurtzorg Model [Internet]. New York: The Commonwealth Fund; 2015 May [cited 2023 Jun 27]. 12 p. Available from: https://www.commonwealthfund.org/publications/case-study/2015/may/home-care-self-governing-nursing-teams-netherlands-buurtzorg-model
- Closing the Gap Healthcare [Internet]. Ontario (CA): CGH; c2020. Care Costs in Ontario—A Complete Breakdown; 2019 May 20 [cited 2023 Jul 20]. Available from: https://www.closingthegap.ca/home-care-costs-in-ontario-a-complete-breakdown/
- Sharkey S, Lefebre N. Leadership Perspective: Bringing Nursing Back to the Future Through People-Powered Care [Internet]. Nursing Leadership; 2017 March [cited 2023 Jun 27]. 30(1)11-22. Available from:
https://www.longwoods.com/content/25110/nursing-leadership/leadership-perspective-bringing-nursing-back-to-the-future-through-people-powered-care doi:10.12927/cjnl.2017.25110

